In an intensive care unit, a burn patient in respiratory distress is almost out of danger. Nurses down the hall keep an eye on his breathing with the help of a non-invasive device that doesn’t require electrodes touching burned skin.
Elsewhere, a premature baby has just gone home, but her parents need to ensure sleep apnea doesn’t last more than a few seconds and deprive her of oxygen. A contactless monitor tracks the rise and fall of her chest, letting her and her parents get some sleep.
And for an older woman receiving care at home, a discreet box near the ceiling of her bedroom monitors her vital signs without requiring her to wear a monitoring device, improving her quality of life.
For situations where conventional cardiorespiratory monitors requiring electrodes and leads would injure damaged skin or prove too cumbersome, a contactless device may fill a vital need, say researchers at the University of Sydney. The team has developed a low-cost, high-resolution radar system that uses millimeter-wavelength signals previously out of reach of any but expensive and unwieldy lab machines.
They published their results early this year in the Laser & Photonics Reviews journal.
David Gubbrud, an emergency room physician at the University of Minnesota Medical Center, says such a device could find utility, especially in cases where conventional electrodes won’t stick. “Heart rate and respiratory rate, to just monitor that on a patient, without having three big wires,” he says, could prove beneficial. Also, “if a person is diaphoretic—drenched in sweat—it can be hard to get those leads to stick on them.”
A fortuitous failure
The new system was borne out of a lucky failure.
The research team had been trying to improve the resolution of aircraft tracking radar systems but found that their new system lacked the necessary range. “It wasn’t particularly good at seeing things at long distance,” explains Benjamin Eggleton, principal investigator for the radar system and director of the University of Sydney Nano Institute. “But that was a blessing more than a curse because it pointed to a really important application: detecting human movement.”
Radar works by sending out radio waves that bounce off a target to return to the receiver. The device processes the return signal to create a picture of the target and gather information about its location, speed and direction. Conventional radar systems are good at resolving large objects like aircraft, but their frequency bandwidth limits the details they can make out.
“Radar signals used at the airport are typically pretty low-frequency because you don’t need to resolve the details of the airplane,” Eggleton explains. “You really just need to know if it’s there or not. As you go to a higher frequency, say 40 gigahertz, which turns out to be harder and harder to do, you can increase the bandwidth.” Greater bandwidth lets radar see more detail but is harder to achieve.
Eggleton and his team had been trying to develop a system to identify different aircraft types of similar sizes and shapes—details lost on conventional radar. That didn’t work because of the range limitations, but they found that they could resolve centimeter-scale details close up. That gave them the idea of adapting their technology for human and animal health applications.
Photonics for high-resolution radar
The key innovation that made close-up, detailed radar sensing possible was the use of photonics—that is, technology that emits, modulates and detects light waves.

Increasing the frequency and bandwidth of radar signals typically requires high-speed electronics with lots of processing power. The required components are large and expensive—too bulky and costly for the applications Eggleton and his team now envision. “Generating these high-bandwidth radar signals is really difficult,” Eggleton says. “You need high-speed electronics. You need big, bulky arbitrary waveform generators. You need signal generators. You need high-speed RF components.”
To reduce the complexity of the electronics in their experimental radar, the team turned to photonics to generate high-frequency radar signals instead of relying on electronics alone.
The photonic components in the system generate light waves. A conventional optoelectronic detector then picks up the light signal and translates it into the high-frequency radio waves needed for high-resolution radar. “We’re doing the generation of the bandwidth signal in the photonics domain, where we have much more flexibility,” Eggleton says. “And the reason we have more flexibility is because the wavelength of the photonic wave is much shorter and the frequency of the photonic wave is much higher.”
The result is a slimmed-down system that Eggleton says he and his team could shrink to a hand-held device suitable for hospitals and other settings out of the laboratory. “It’s a reconfigurable broadband radio wave generator that I can use to image with incredibly high spatial resolution without using any high-speed electronics,” he says.
Cane toads and prototypes
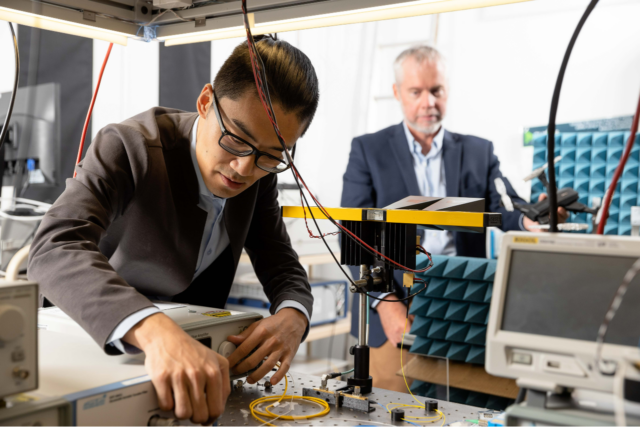
Eggleton says his team’s experimental radar system exists only as a tabletop, laboratory prototype, for now. But, he says, it can track the rise and fall of a person’s chest as they breathe, even through clothing and blankets. And since it doesn’t rely on cameras, it can’t capture faces or “naughty bits,” preserving privacy.
Next steps for the team include further refining the system, hopefully to the point where it can monitor heart rate as well as respiration, and testing it on animal subjects—cane toads to start. “We need to demonstrate in a real-world setting that we can separate the vital signs from all the background noise,” Eggleton explains. He says he’s in talks with potential commercial partners to fund the development of a medical-grade, smaller-size version of the prototype for further testing.
Any time you get a new technology, there are equipment costs, and you have to teach people how to use it. You want to make sure if you’re going to put that effort in, it’s going to be a game-changer.
—David Gubbrud, emergency room physician, University of Minnesota Medical Center
Among the challenges Gubbrud sees in any potential clinical setting is getting healthcare organizations and professionals to adopt it. “Any time you get a new technology, there are equipment costs, and you have to teach people how to use it,” he says. “You want to make sure if you’re going to put that effort in, it’s going to be a game-changer.”
Despite the challenges, co-lead researcher Ziqian Zhang, a Ph.D. candidate at the University of Sydney, expressed optimism in a university press release. “We hope to see real-world applications of this low-cost technology in the not-too-distant future.”
Lead photo courtesy of Shutterstock

