By Anne Miller, Contributor
Photos by Jeff Wilson
Slowly, and amid the soft hum of small motors, Avrel Seale began conducting Beethoven’s Symphony No. 5.
“My dad was an orchestra director,” says Seale, 52, a staff writer in the communications department at the University of Texas at Austin. “I thought about him as I [conducted].”
YOU MAY ALSO LIKE: How AI Helps Give ALS Patients a Voice
One afternoon in 2018, Seale suffered a debilitating stroke while in his office at UT. Brain surgery followed, and he remained hospitalized for 10 weeks. Afterward, he had to relearn how to walk and regain movement in his arm and hand; his right arm and leg were partially paralyzed. Today, Seale cannot open his right hand completely.
About six months after his stroke, Seale strapped his arms and shoulders into a Harmony robot in UT’s ReNeu Robotics Lab. He was told the experimental rehab technology probably wouldn’t help him much—though experts say the first few weeks are key to recovery. Still, Seale decided to participate in the trial, not for himself but for future stroke patients who might benefit from the new technology.
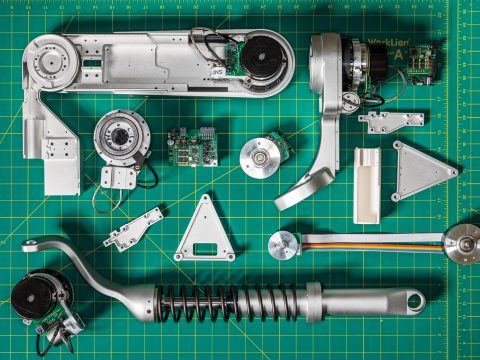
For 12 weeks, Seale worked with the upper-body exoskeleton, built to augment the physical and occupational therapy that stroke victims endure to regain control of their upper bodies. Harmony, with a white plastic outer casing and metallic connectors and pieces, resembles something out of a Star Wars movie.
The Harmony exoskeleton employs sensors and custom controls to help patients relearn movements. The system gauges when a patient’s movement needs less or more support. As the human brain starts to rework connections and the arm muscles conduct more work, Harmony backs off just a little, adjusting to encourage the wearer’s musculature. For instance, during one session, the patient may mimic picking up a pencil; if the patient struggles, the robot will take charge, reminding the body of how a natural movement feels. Therapists can then track progress and set parameters via the easy-to-use touchscreen interface.
On the last day of Seale’s testing, the ReNeu team engaged a mirror setting: Seale moved his good arm and the robot would lift his other arm in tandem, with mechanics supporting the shoulder, elbow, and wrist. Seeing and feeling his injured arm move almost naturally for the first time in months triggered deep emotions and channeled the conductor memories of Seale’s youth.
Some of the nation’s leading physical therapists hope Harmony represents a breakthrough not only in stroke rehabilitation but also in the role technology can play in supporting health therapies and our bodies.
10,000 Movements
The mastermind behind the Harmony robot, UT robotics professor Ashish Deshpande, Ph.D., has spent nearly a decade learning from neuroscientists and the medical community to advance his creation.

Robotics for lower body therapy have existed for years, but the upper body presents a deeper challenge. To help a person walk, a machine moves front to back—and maybe up and down. The upper body has a much broader range of motion, and engages more joints.
Deshpande’s inspiration for solving this challenge came when he broke his hand playing ultimate frisbee as a student years ago, which led to the discovery of a benign tumor in his hand, and weeks in therapy regaining his full range of motion after surgery. His sister, a physical therapist, offered guidance on therapies and sparked curiosity in Deshpande. Could he apply robotics to physical therapy?
According to the Centers for Disease Control, more than 795,000 Americans suffer a stroke every year, and the costs associated with strokes, including treatment and missed work days, total more than $34 billion annually.
Dr. Robert Lee, medical director of stroke and neurological recovery at St. David’s Rehabilitation Hospital in Austin, Texas, says repetitive motion remains key to recovering range of motion after a stroke, but the time and repetition involved can be daunting.
“For stroke rehabilitation, one of the most important principles is neuroplasticity—basically the brain’s ability to adapt and rewire to new experiences with training,” he says. “It takes about 10,000 repetitions to retain a skill. If you’re trying to pick up a pencil efficiently, you need to practice that about 10,000 times before the brain is able to rewire itself to do that efficiently.”
Assuming a therapist can assist in a movement 100 times in an hour-long appointment, a patient would need more than 100 hours of therapy, Lee explains. Health insurance like Medicaid limits therapy visits, which can further reduce the exposure to repetition. But a robot could boost those repetitions to 500 per hour.
Five hundred may seem like a lot, especially for a patient struggling with weak muscles, Lee admits. “[But] I don’t believe there is a limit to what the patient can tolerate as long as we do it in a safe, controlled, supported way.”
St. David’s, along with Good Shepherd Rehabilitation Network—two prominent rehabilitation centers in the U.S.—are poised to run tests with patients and the Harmony exoskeleton early this year.
“Stroke causes death or damage to your brain, part of your motor cortex,” says Frank Hyland, executive director and administrator of Good Shepherd Rehabilitation Network, based in Allentown, Pennsylvania. “It’s bad enough when you have a stroke that you have some initial paralysis or weakness. But if you don’t use your muscles the natural way, that weakness will get worse.”
This natural movement proved most difficult in Deshpande’s creation of Harmony. “I came in thinking that we have a full knowledge of how people recover, and with my robotic knowledge, I [could standardize]—maybe automate—that type of recovery,” Deshpande says. “But there are many open questions in the medical field … I really had to use my robots as tools to discover how people recover, and then use them as therapy tools.”
A Repetitive Motion Machine
One of the biggest challenges Deshpande faced involved adapting the robotics to a human body. Motors created for the rapid installation of heavy car parts on an assembly line, for example, couldn’t gently support the raising and lowering of a human arm. Deshpande and his team had to design and build their own parts of motors and ball bearings in order to achieve the smooth operation and light touch needed to support—but not overpower—the movement of a human shoulder.
“A lot of controllers are designed for [speed] and accuracy—we needed one designed for the human interaction,” says Deshpande. “On a human … we need accuracy,” he says, “[but] what we need most is safety and comfort.”
“The only way you learn is you fail and try again, you fail and try again,” Deshpande says. “Physical therapy [works] the same way a child learns to walk. It’s the way we learn any new task. We try, we learn, we get that data. This is relearning the action the person used to know, but—because they have brain damage—they have to relearn.”
Deshpande, with business partner and now CEO Christopher Prentice, has spun off a commercial development company, Harmonic Bionics, Inc., to bring Harmony to market. While the price point has yet to be determined, it is likely a cost that only a hospital could afford, which could limit the number and location of patients with access.
Prentice sees automation as the future of rehab—it’s not a question of when but how, he says. And who will get there first.
“I was really impressed to what stage they got it to within an academic lab,” says Prentice. “[No existing systems] treat the scapula all the way up the shoulder with the range of motion that Harmony does.”
Hyland, at Good Shepherd Rehabilitation, agrees. “I think it’s going to be a game-changer.”